HINT: When to worry and how to assess for symptoms of COVID-19 in congregate/community settings?
Connected Care Quick Hits are up to date and evidence based recommendations for the care of children with medical complexity & technology dependence, from hospital to home.
HINT: When to worry and how to assess for symptoms of COVID-19 in congregate/community settings?
SITUATION:
This week’s QuickHit! comes from a community health care provider working with children and families living in a congregate setting, who asked about how to screen and recognize which children/youth may be presenting with new and worrisome signs and symptoms of COVID-19.
BACKGROUND:
It is clear that children compared to adults have a low infection rates of COVID-19. Among these, children typically experience mild disease with many being asymptomatic.
While severe disease and deaths from COVID 19 in children are rare, they continue to be reported around the world. Being under the age of 1 is a risk factor for severe/critical disease. Less is known about the potential heightened risk for children with underlying medical conditions. Children living in congregate/community settings may be at increased risk for contracting COVID-19 and health care providers working in these settings are well positioned to partner with children/youth and families to monitor for symptoms and identify any signs of serious disease.
Symptoms of COVID-19 in children include typical (common, expected) and atypical (uncommon, unexpected) presentations of the disease and differ from typical presentation in adults.
Note: Evidence and experience with COVID-19 in children is constantly changing. This information was prepared based on best evidence available June 4.
ASSESSMENT:
When caring for a child with known or suspected COVID-19 in home/community, a systematic and step-wise approach to assessment may aid in early identification of signs and symptoms of mild disease and signs of suggestive of worrisome or serious disease. Tools that support peadiatric health assessment that are easy to use in congregate/group/home care settings are described here:
1. CLINICAL STATUS: The Paediatric Assessment Triangle (PAT) is an observational tool guides a rapid assessment of the child’s overall clinical status to help direct initial clinical management priorities. It can be completed in <1 mins with no equipment necessary as it relies on the ability to ‘eyeball the child’. For more information on how to complete the PAT see: Connected Care QuickHit: How to do the PAT?
2. SIGNS AND SYMPTOMS OF COVID 19: After confirming the child’s clinical status is stable, the use of a checklist such as the one below, promotes child/family self-reporting any new or progressing symptoms of COVID-19. Symptoms most often seen in children are:
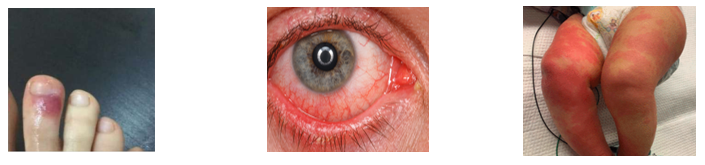
Inflammatory changes in children may be atypical signs of COVID-19 and include persistent fever and skin/integumentary changes that may look like this:
Consejo Genral de Colegios Oficiales de Podologos de Espana. Registro De Casos Compatibles COVID-19. Available from https://cgcop.es/2020/04/09/registro-de-casos-compatibles-covid-19/?fbclid=IwAR2wv4ocR2eLQGPVSChBuPeDjub6Ay7tAZwqiuWISwYe0EqCPPklhRb3Rdg. Accessed 21st April 2020
More pictures available at: https://hosppeds.aappublications.org/content/10/6/537.long
3. VITAL SIGNS: After observing the child’s clinical status, and completing the self-reported symptom checklist, if there is concern or worry for the child’s health, vital signs may be a helpful in assessing a child’s risk for serious disease. In otherwise healthy children, routine vital signs typically include only temperature, heart rates, and respiratory rates. Blood pressure and oxygen saturations are added to the assessment of vital signs if and when there is heightened concern for a child’s health status.
Consider typical ranges for child’s size/age, and use age appropriate techniques to take the vital signs.
RECOMMENDATION:
For this consultation, Connected Care suggested that health care providers assessing a child in any congregate, shelter or community/home care setting:
Monitor routinely and consider testing for presence of new or progressing symptoms of COVID 19
Seek urgent medical attention if: Any child appears at all unwell as per the PAT assessment
Any infant < 3 mos of age has a fever
Any child displays sign of systemic inflammatory disease (red eye, skin changes)
The child has any sign of medical instability (vital signs deviate from child’s baseline [tachypnea, tachycardia] or are outside of typical range for child’s age, lethargy)
Any time the child/family/provider are concerned or worried about the child’s health condition
Call 911 if:
The child is in respiratory distress, shows signs of impending cardiovascular collapse, displays an altered neurological state OR anytime there is heightened concern or intense worry.
For trusted information from AboutKidsHealth to share with families click here to visit the COVID-19 Learning Hub
Have a Question? Initiate a Consult!
Connected Care Live is not to be used in the event of an emergency.