HINT: What is the correct catheter size when suctioning a tracheostomy?
Connected Care Quick Hits are up to date and evidence based recommendations for the care of children with medical complexity & technology dependence, from hospital to home.
HINT: What is the correct catheter size when suctioning a tracheostomy?
SITUATION:
This QuickHit was informed by a Connected Care Live consult from a Community/Home Care Provider asking about the most appropriate size suction catheter to use for a child with a tracheostomy.
BACKGROUND:
Tracheal suctioning is indicated for children with artificial airways:
to remove secretions from the child's upper airway
to maintain a patent upper airway and prevent obstruction
to avoid aspiration of food and/or liquid from the upper airway
The size of the suction catheter, depth and duration of suctioning, as well as the pressure used makes a difference in the effectiveness of this routine intervention.
ASSESSMENT:
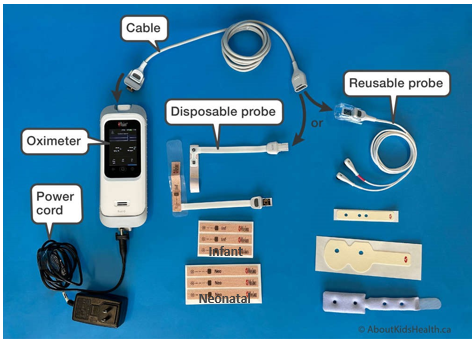
At the start of each shift, complete a safety check to assess all equipment is functioning and tracheostomy supplies are on hand. Plan for the child's routine tracheostomy care and be ready for emergencies.
Tracheostomy care requires continuous assessment for signs that may signal the need for tracheal tube suctioning:
Auscultation: coarse crackles detected.
Visual/audible cues: active coughing with inability to clear secretions, audible upper airway congestion or visible secretions.
Respiratory distress: increased respiratory rate, irritability, work of breathing or shortness of breath thought to be related to secretion retention (i.e. unexplainable by another reason such as exertion).
Oxygen saturation decrease or increase in oxygen requirements
Ventilation changes: sporadic flow waveforms, lower tidal volume, or higher peak pressure.
RECOMMENDATION:
When performing suctioning on a child with a tracheostomy, consider the following :
Size of suction catheter
The recommended suction catheter is based on the size of tracheostomy tube:
If the suction catheter is too large, it may occlude the tracheostomy tube and cause difficulty in breathing.
If the suction catheter is too small, it may impair effective clearance of the secretions.
2. Depth of suctioning
Tip suctioning – removes mucus or fluids at the very front of the tracheostomy tube. Suction catheters and tip suction devices may be used for tip suctioning (e.g. Little Suckers®)
Tube suctioning - removes mucus or fluids from the full length of the tracheostomy tube, including just past the far end of the tube. The appropriate depth is to be pre-measured. If you are unable to insert the whole pre-measured length, this may be an indication that the tracheostomy is blocked and needs to be changed.
Deep suctioning – removes mucus or fluid from the child's airway beyond the tube. This is typically only performed with orders from the child's prescriber (MD/NP).
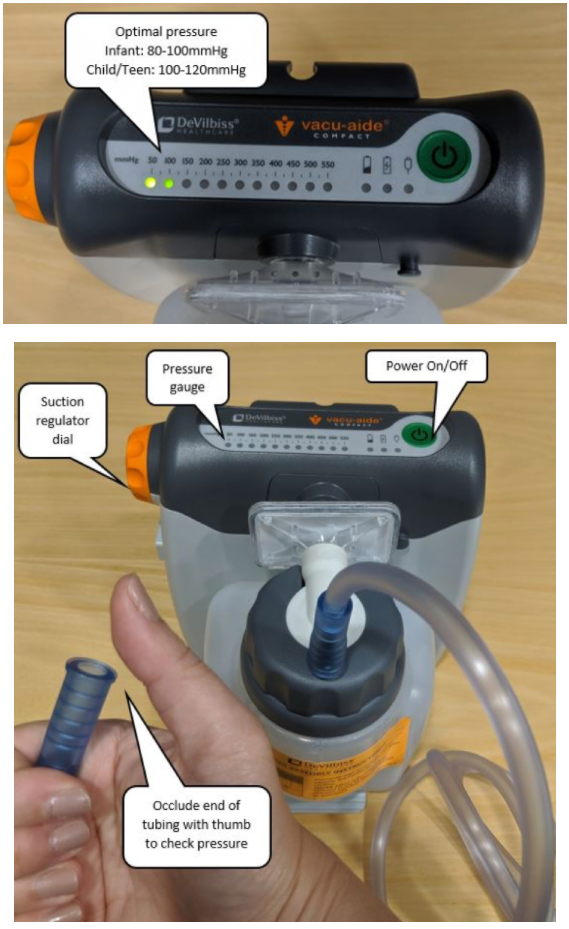
3. Pressure setting on suction machine
Check that the suction machine is set according to what the child's family caregiver and health care team recommends. These settings enable good pressure for secretion clearance and limit potential trauma to the airway and are typically within these ranges:
Infant : 80-100 mmHg
Child/Teen: 100-120 mmHg
To learn more about how to check for the right pressure click here to see our QuickHIT.
Check the suction pressure at the start of your shift as part of your initial safety check, as well as every time you use the suction machine on a shift.
For more information about suctioning visit AboutKidsHealth
Connected Care Live is not to be used in the event of an emergency.