HINT: How to manage the cuff of a paediatric tracheostomy tube
Connected Care Quick Hits are up to date and evidence based recommendations for the care of children with medical complexity & technology dependence, from hospital to home.
HINT: How to manage the cuff of a paediatric tracheostomy tube
SITUATION:
This QuickHit was informed by a Connected Care Live Consult from a community/home care provider that prompted teaching about cuffed tracheostomy tubes
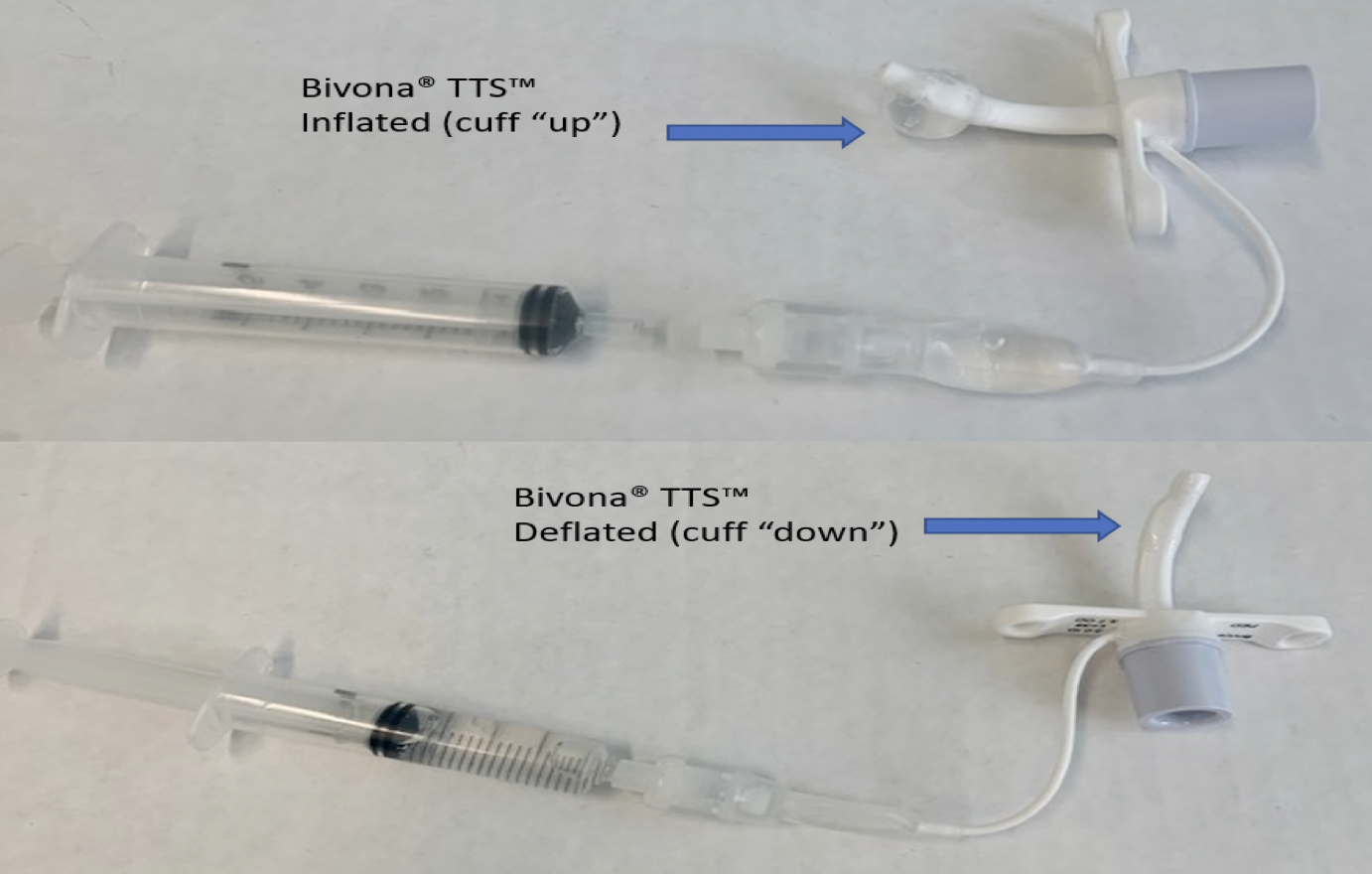
A pilot balloon which sits outside the airway is used to fill the cuff. When the pilot balloon is deflated, this indicates that the cuff is deflated and vice-versa.
BACKGROUND:
Paediatric tracheostomy tubes may be a cuffed or uncuffed. The purpose of a tracheostomy cuff is to maintain the air delivered from the ventilator to the lungs, improving ventilation. When the cuff is inflated, it fills the tracheal space around the tracheostomy tube to prevent airflow from escaping around the tube and up through the vocal cords and into the mouth and nose (‘leaking’).
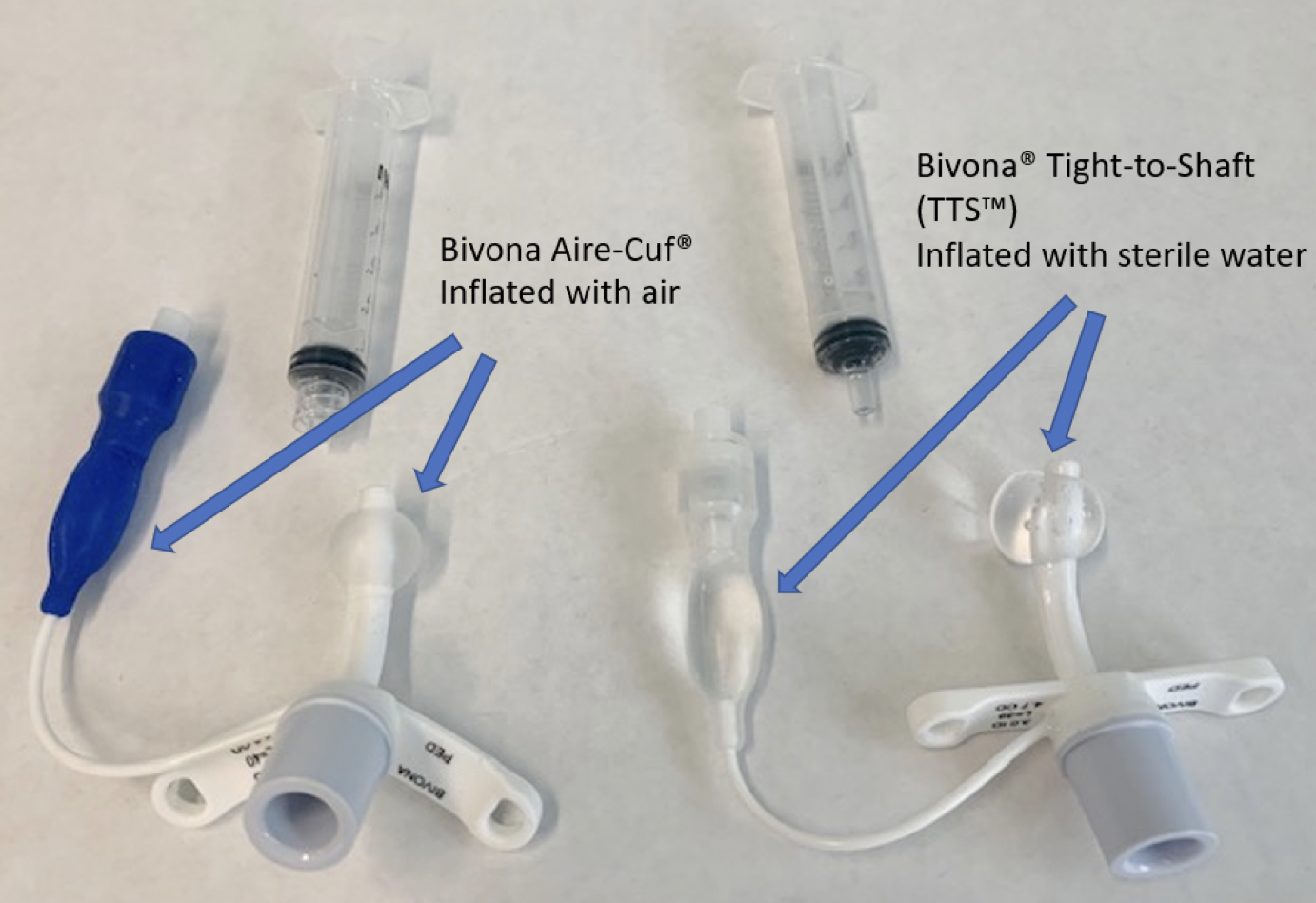
A cuffed tube has a balloon-like feature at the distal end of the tube. This cuff can be filled with air or sterile water depending on the type of tracheostomy tube. The amount of air or sterile water placed into the cuff is prescribed as well as when the cuff should be inflated vs. deflated.
ASSESSMENT:
When caring for a child with a cuffed tracheostomy tube, the home and community care provider will verify complete orders, which include:
Type of cuffed tracheostomy tube
Volume prescribed to inflate cuff
What to fill cuff with - air vs. sterile water
Child's schedule - when to inflate/deflate
Any ventilator changes required with cuff use
When does the cuff need to be inflated?
Before initiating ventilation as prescribed (e.g., before sleeping)
With cough assist therapy
When does the cuff need to be deflated?
Prior to a tracheostomy tube change
When child is awake as prescribed
For communication or with a speaking valve
After cough assist treatment is completed
RECOMMENDATION:
Be prepared to manage a child's cuffed tracheostomy tube by:
Understanding indications for cuff
Reviewing complete orders
Partnering with family caregivers to understand child's routine with their cuff
Practicing using the cuff, to be ready for emergencies (e.g. unplanned tracheostomy changes)
At the beginning of each shift, verify the correct amount of air or water in the cuff by completing the steps below:
Steps to Deflating a Tracheostomy Cuff
Before starting, ensure:
A medical order is in place
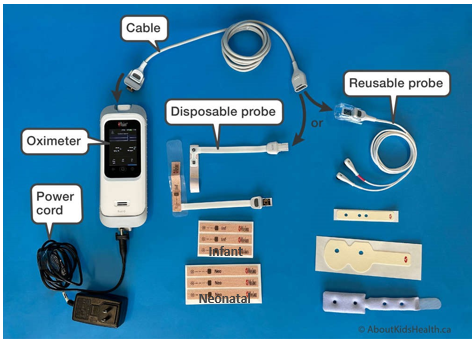
Cardiorespiratory monitoring (i.e., oximeter)
Client has not just eaten
Client is stable
Emergency equipment and supplies are available
Appropriate PPE is worn
Empty syringe (slip tip or luer lock) is available
Steps
Tube suction patient, orally suction if needed
Stabilize pilot balloon between fingers and attach the syringe
Slowly pull back on syringe to empty the pilot balloon until flattened
Tube suction again, orally if needed
Monitor for any signs of distress
Make note of the amount of water retrieved from cuff
Steps to Inflating a Tracheostomy Cuff
Draw up correct amount of air or sterile water (depending on the trach cuff type) in syringe
Attach syringe to the pilot balloon and slowly inflate to the prescribed amount
Suction client if cuff inflation triggers a cough and secretions
Make note of leak value on ventilator.
If leak value progressively increases, recheck cuff by following the deflation and reinflation steps.
If leak continues or if pilot balloon does not remain inflated, inform family so you can plan to change the tracheostomy tube.