ALERT: What are safety considerations for children with nasogastric (NG) tubes?
Connected Care Quick Hits are up to date and evidence based recommendations for the care of children with medical complexity & technology dependence, from hospital to home.
ALERT: What are safety considerations for children with nasogastric (NG) tubes?
SITUATION:
This Quick Hit was informed by family caregivers and home and community care providers that have inquired about safety considerations for children with NG tubes in home and community settings.
BACKGROUND:
Children with medical complexity may rely on NG tubes to support nutrition, hydration, and/or medication administration. With the increasing use of NG tubes in home and community settings, there are important assessments and considerations to ensure safety of children and to prevent complications such as aspiration, tube migration and dislodgement.
ASSESSMENT:
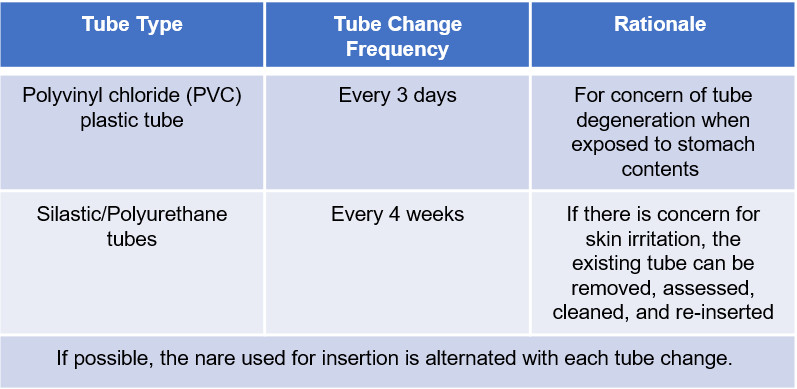
There are two types of NG tubes commonly used for children in hospital, home and community settings. Each type of tube has specific recommendations for frequency of changes, as outlined in the table below.
Routine assessment of the placement of NG tubes before their use supports verification that the tube remains in the stomach and is safe to use. Placement of the NG tube is to be assessed:
Before the tube is used for feeding/medications
When a new tube is inserted
If there is a concern that the tube has been pulled or changed position
The child has signs of vomiting, coughing, choking, or change in breathing
Every 8 hrs during a continuous feed
Placement of NG tubes can be verified by X-Ray and/or assessing the pH of stomach contents aspirated from the tube.
Auscultation and listening for a “pop” is NOT a recommended method of confirming NG placement.
RECOMMENDATION:
Connected Care recommends the following safety assessments and considerations when caring for children with NG tubes in home and community settings:
Constant observation during feeding administration and/or medications through the NG tube for the following populations:
Any child based on neurodevelopmental age, delays, or impairment that does not have the ability to recognize and/or communicate to their caregivers if they experience issues with the NG tube (e.g. entanglement, displacement) or NG feeding (e.g. vomiting)
Absence of a gag reflex, known or suspected aspiration with liquids or other inability to protect their airway
Use of Non-Invasive Positive Pressure Ventilation (NIPPV) while feeding through the NG tube
Consideration for the patient position during feeding through the NG tube
Developmentally appropriate positions/alertness for mealtimes (e.g., in highchair at a table with family, ensure the child is awake, if feed is taking place during daytime hours or unless otherwise discussed/recommended by your care team)
Promoting safe sleep practices
Use of a car seat during feeding may not be appropriate as it can increase abdominal compression which could lead to vomiting or feeding intolerance
Consideration for practices to reduce the risk of dislodgment, entanglement, and strangulation at home
Positioning the enteral feeding pump at the end of the bed instead of the head of the bed to keep the tubing and NG tube away from the child's head and neck
Thread the NG tube through the clothing of a child (e.g., through the length of a onesie or sleeper for an infant and have the tube coming out the bottom)
Coil the external length of the NG tube and use tape to secure it to the back of the shirt of the child.
The type and amount of water used to flush the NG tube is dependent on a variety of factors, including:
Sterile water is recommended for children under 4 months of age
Tap, well, bottle, distilled, or sterile water can be used for children over 4 months of age.
Avoid sweetened, vitamin-enhanced, flavoured, or carbonated water for flushing
The length of formula hang time (the amount of time out of the fridge or opening of a shelf stable product) can differ:
Spiked closed system up to 24 hours
Decanted ready-to-feed formula up to 8 hours
Reconstituted powdered formula up to 6 hours
Reconstituted liquid concentrate up to 6 hours
Human milk +/- fortifier or powdered formula up to 4 hours
The preferred method of delivery for feeds through an NG tube is via gravity or syringe. Feeds may be delivered via a pump if the child is unable to tolerate gravity or syringe feeding.
Review the following AboutKidsHealth articles about caring for children with NG tubes.
At this time, Connected Care Live is limited to home and community care nurses and pre-registered family caregivers, and is not to be used in the event of an emergency.